
Nancy Green, senior vice president at Aveus, sat down with Julie Barnes, founder of Maverick Health Policy, and Debbie Hill, vice president of product management at Medecision, to discuss changes that the Centers for Medicare & Medicaid (CMS) has made to Star Ratings—and what it means for Medicare Advantage programs and health plans.
By Nancy Green, Senior Vice President, Aveus
At the end of June, I had the opportunity to sit down with Julie Barnes, founder and principal of Maverick Health Policy, and Debbie Hill, vice president of product management at Medecision, for an insightful discussion about changes to the Centers for Medicare & Medicaid (CMS) Star Ratings System—and what these changes mean for Medicare Advantage (MA) programs and health plans.
But first, a little background: The Star Ratings launched in 2007 as a way for CMS and Medicare beneficiaries to assess and compare MA plans. Ratings range from one to five stars, with five the highest score and one the lowest. In theory, the higher the score, the better the plan.
In 2012, as part of the Affordable Care Act, CMS began rewarding plans with higher ratings with financial incentives. These financial incentives made a big difference—encouraging health plans to improve their scores by improving outcomes. As a result, enrollment in these plans also increased. But the ultimate key to a high score is data collection—meaning that data from HEDIS (Healthcare Effectiveness Data and Information Set) and CAHPS (Consumer Assessment of Healthcare Providers & Systems) reporting really matters.
“HEDIS is a standardized set of performance measures,” Barnes explained. “HEDIS measures relate to many important public health issues, such as cancer, heart disease, smoking, asthma and diabetes. CAHPS is an annual survey that is used for rating a patient’s healthcare experience.”
Star Ratings Put Greater Emphasis on Experience
In May 2020, CMS revised the Star Ratings system to put a greater weight on the results of the CAHPS survey. By 2023, the consumer experience will determine 57% of overall star ratings.
So why did CMS decide to place a greater emphasis on member experience and engagement? What sparked the change? According to Barnes, there’s an interest in improving the overall experience for consumers right now.
“This change is in keeping with the overall idea that if you improve the member experience to empower patients, they will make better healthcare decisions,” Barnes said.
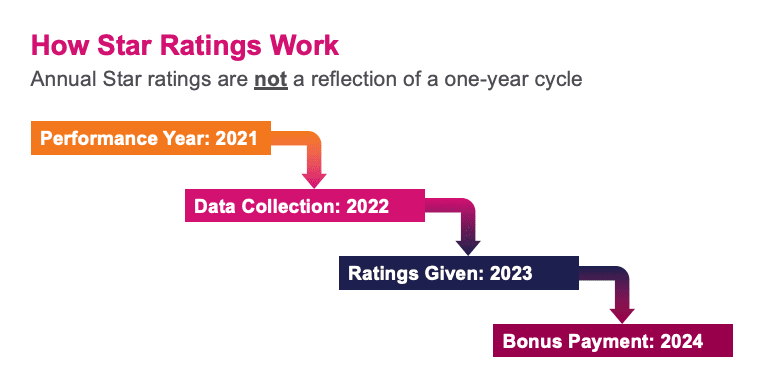
Based on the timing of surveys, consumers will be asked about their perceptions of their health plan beginning in late 2021. It’s important to note that Star Ratings are not a reflection of a one-year cycle, Hill added. For example, if 2021 is the performance year, then data collection occurs in 2022, ratings are given in 2023, and bonus payments are issued in 2024.
“With respect to the 2021 rating calculations and the impact of the pandemic, CMS will use the scores from 2020 for the 2021 ratings,” Hill said. “However, if the pandemic continues to prevent the agency from having validated data, CMS will replace 2019 data that was gathered in 2020 with the Star Ratings and score from 2020. It’s complicated, for sure, but CMS is trying to take into account the implications of the pandemic in 2020.”
What Changes Mean for Medicare Advantage Plans
As explained earlier, the Star Ratings are awarded on a five-star scale, with five stars representing the highest quality. Each plan providing health coverage, such as Medicare Advantage or Medicare Cost, is given an overall summary rating based on how it performs across five main categories:
- Staying healthy: Plans are rated on whether members had access to preventive services to keep them healthy. This includes physical examinations, vaccinations and preventive screenings.
- Chronic conditions management: Plans are rated for care coordination and how frequently members received services for long-term health conditions.
- Member experience: Plans are rated for overall member satisfaction with the health plan.
- Member complaints: Plans are rated on how frequently members submitted complaints or left the plan, whether members had issues getting needed services, and whether plan performance improved from one year to the next.
- Customer service: Plans are rated for quality of call center services and processing appeals and new enrollments in a timely manner.
For Medicare Part D standalone plans or Medicare Advantage plans that include drug coverage, ratings are based on member experience, member complaints, customer service, and drug safety and drug pricing accuracy, Hill said.
Highly rated plans (4+ stars) are awarded quality bonus payments—financial incentives for achieving a high rating. High-performing plans also gain advantage in the marketplace with no member enrollment restrictions. Despite being a component of the Star Ratings criteria for years, health plans have historically not been successful in improving the member experience. Now, with a greater emphasis on the overall experience, that will have to change.
“Consumers are more technologically savvy today,” Hill said. “They know how to look up the information on their plan’s overall performance and they are using that information to make informed decisions about their healthcare.”
To hear more from my conversation with Julie Barnes and Debbie Hill, click here to access the webinar.
Editor’s Note: On August 5, 2021, CMS announced that two Health Outcomes Survey (HOS) outcome measures, Improving or Maintaining Physical Health and Improving or Maintaining Mental Health, will be removed from 2022 and 2023 calculations due to COVID-19. Learn more here and here.



About The Author: Nancy Green
Nancy Green is Senior Vice President of Aveus, the consulting and professional services division of Medecision. Nancy has deep experience and strategic partnerships in the healthcare ecosystem, and leverages her technology and healthcare industry expertise to define strategies, drive innovation, and stimulate growth for her clients. She is passionate about improving organizational agility and helping leaders become bolder in their decisions.
More posts by Nancy Green