
In April, Dr. Terry McInnis explained what researchers were learning and studying about the coronavirus. Now, five months later, Dr. McInnis shares even more information about testing, the risk of exposure and the severity of the disease.
By Terry McInnis, MD, MPH, CPE, national expert on preventive medicine and integrated medication management
It’s hard to believe that August is almost over. In March, as the coronavirus began to spread rapidly throughout the nation, many people thought that the worst would be over by fall and we could resume our normal lives. Now, as we inch closer to September, many of us have settled into a “new normal”—donning masks every time we are around those not in our “bubble”, carrying bottles of hand sanitizer with us in our bags, ordering takeout instead of dining in at restaurants, and adjusting to work-from-home routines. It also has had the silver lining of making us pause—and perhaps begin to take inventory of our many blessings.
In my last blog post, published in April, I explained what experts knew about the coronavirus thus far—and what they were continuing to study. Now, in August, as worldwide cases have soared past 20 million, researchers are getting a better grasp on COVID-19 and how it is spread and how it affects different people.
There’s been a lot of debate and confusion over the past six months about how the virus is spread—and whether masks are important. It’s clear now, however, that the virus is spread through airborne aerosol, similar to how SARS was spread in 2002–2003. But it’s not just spread through coughing and sneezing—simply talking in bars, restaurants or around other people in enclosed environments (like churches) can infect people. This is just more evidence that continuing to practice social distancing and wearing a mask when in enclosed spaces are incredibly important.
One thing that researchers have reconsidered, however, is how often the virus is transmitted through contact. Although it continues to be important to wash your hands and avoid touching your face, we’re not seeing many people get COVID-19 from the mail, their groceries or takeout food. It’s still important to think about high-contact areas like door handles, keypads and gas nozzles, but to be completely honest, I’m not as worried about checking my mail, opening a package or handling the bags of groceries as I once was.
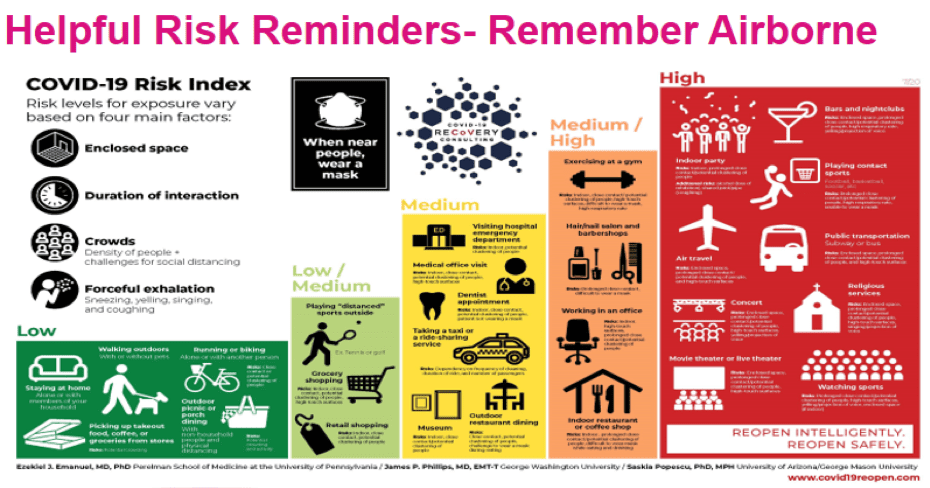
Risk levels for exposure vary, based on four main factors: enclosed space, duration of interaction, crowds, and forceful exhalation (although simply breathing and speaking is enough). Get outdoors and walk and exercise—it helps both mentally and physically!
Understanding Testing and Immunity
As I explained in April, there are two types of tests for the coronavirus. The first is the reverse transcription PCR (polymerase chain reaction) test, which actually tests for the presence of the virus in the body. This test isn’t perfect, however, and depending on when in the course of the virus you are tested, and if you sample enough live virus, it can be falsely negative. If you’ve been tested and the results come back negative but you have symptoms that are consistent with the virus—especially loss of smell and taste—it’s safer to consider yourself positive and quarantine appropriately.
Researchers are also looking at more availability of home testing and testing in the workplace—with immediate results—and at a cheaper price point. Some of the tests will have color indicators or a plus or negative sign for easy interpretation, like pregnancy tests.
There’s also the antibody test, which is conducted through a blood sample and looks for the presence of antibodies. It tests whether your body has responded to the infection and produced antibodies specific to the virus, not whether you are currently infected. We are still learning more about immunity to the virus.
Your immune system is divided into two subtypes. The first is called the innate immune system—the first line of defense. Your innate immune system is capable of detecting viruses and bacteria as soon as they enter the body, and it responds quickly. It doesn’t always get rid of infectious organisms and pathogens, but it does cue the adaptive immune system to kick in. The adaptive immune system is slower and can take more time (sometimes one or two weeks) before two important types of cells—B cells and T cells—get to work. T cells are grouped into two subtypes: CD4+ cells are helper cells that release cytokines that produce B cells, which create antibodies. CD8+ cells are cytotoxic T cells, which kill infected cells.
What we’re beginning to see is that our bodies have what’s called a T-cell response. Essentially, once the virus enters your body, your immune system remembers it because it has developed the T cells that can quickly go and attack it if it enters again.
When talking about immunity, you may have heard the phrase “cytokine storm.” This happens when a patient’s immune system has declared all out war to stop the virus- think of a nuclear blast. The problem is that the body’s defense system then harms its own cells and tissues, rather than just fending off the virus. Medications such as dexamethasone- a steroid, however, help tone down the immune response so that it doesn’t overwhelm the body. If we tone down our immune system (recall the troops) too soon, the virus may win, so when we give drugs like dexamethasone becomes critical. This is another point—some drugs work at different stages of the disease, and some look promising in the lab, but don’t work in the complexity of the body—like what we have seen with clinical trials of hydroxychloroquine.
Who Is at Risk of Severe Disease?
As we’ve seen more confirmed cases over the past several months, researchers have begun to identify who is at a higher risk. Of course, as we’ve known from the beginning, adults 65 and older are at a higher risk. We also see that men and people of color have a higher risk, as do people with comorbidities such as obesity, hypertension, cardiovascular disease, diabetes, chronic obstructive pulmonary disease and lung problems.
Health science company ZOE, in collaboration with scientists from King’s College of London and Massachusetts General Hospital have developed a COVID-19 symptom tracker app with more than 4 million subscribers. It is a great way to learn more directly from people—sign up and you get a text daily asking if you are sick or healthy. It is a great way to join the fight and contribute to the knowledge. Harvard researchers, and others, have started to cluster symptoms together to track the symptoms reported and to see which symptoms require additional support including respiratory support and rate of hospitalizations. This really helps when we are now monitoring more people from home to know which of the 6 symptoms clusters will need higher degrees of support.
Understanding these different levels of severity with symptoms is important, especially as we think about care and case management. Whom do we need to closely monitor, especially when we’re trying to do more monitoring at home? Who’s at a higher risk of low oxygen levels? These are questions we have to consider when looking at symptoms.
Also, we need to understand that this is not just a respiratory and lung disease. COVID-19 infects the lining of our blood vessels and so we are seeing heart inflammation, strokes, thyroid problems, kidney disease, fatigue, hair loss and many other problems. The long-term consequences of this disease, even in mild cases and healthy people, is very concerning. We are also seeing more people with symptomatic disease having a prolonged course of illness—some calling themselves “long-haulers.”
Staying Healthy During a Pandemic
So how does one stay healthy in the midst of a global pandemic? For starters, wearing a mask and practicing social distancing remain the best two ways to stay healthy. There’s also a lot of evidence that adequate levels of vitamin D are very important. Some experts recommend blood levels between 40-60ng/ml (different from nmol/L if you start googling). Since few foods are naturally rich in vitamin D, and it is very hard to get adequate levels from time outdoors (without sunscreen), adding supplements at a responsible level is something that’s easy to do and not harmful to the majority of people. For adults, getting blood levels can be helpful to determine what is right for you. Generally, the recommendations are to stay below 4000IU per day in adults of D3. If you have conditions such as hypercalcemia (sarcoidosis—too high calcium in your blood) or hypercalcuria (kidney stones), you may need to avoid supplementing with D. Lower vitamin D levels may be one factor in why we are seeing more people of color with severe disease—they typically have lower levels of vitamin D. Research also supports healthy levels of zinc and selenium to enhance your immune response and help clear some of the “oxidative free radicals” that can build as your immune system fights.
If you have conditions such as hypertension or diabetes, keep them under control. Continue eating healthily and exercising on a regular basis. It doesn’t hurt to get adequate levels of vitamin C daily either. Do your research on what supplement level may be right for you.
Also, gargling makes a lot of sense. There were three commercial mouthwashes tested that killed the virus after 30 seconds in the mouth and oral cavity—the ingredients in Listerine Cool Mint were one of them. That promotes a 99.9% reduction in bacteria and germs. The virus can stay around in the oral cavity, and gargling (not swallowing) can help at least reduce the load (not cure or destroy the virus already in your cells), so that you don’t transmit as much when speaking.
As more research is conducted and scientists around the world work to develop a vaccine, we’ll learn even more about this novel coronavirus. Until then, continue to be vigilant about your health and do what you can to mitigate your risk.
Hear More on The Liberation Lab Podcast
Want to hear more? Check out Dr. McInnis’ podcast episode on COVID-19 facts and prevention strategies. Look back to Dr. McInnis’ perspectives from the early days of the COVID-19 pandemic.


About The Author: Terry McInnis MD, MPH, CPE
Dr. Terry McInnis is President of Blue Thorn Inc. health care consulting where she advises more than 100 companies and health systems ranging from universities to analytic firms, health plans and pharmaceutical manufacturers. Previously, as business lead for value-based care at LabCorp, Terry set the strategy and built internal capabilities to execute and partner with providers to align diagnostic analytics and clinical trials with better outcomes and lower costs. Terry’s 30 years of experience spans practice, executive and consulting roles. Her military health roles include Chief of Flight Medicine at Patrick Air Force Base and four years on active duty during Operation Desert Shield and Operation Desert Storm.
More posts by Terry McInnis MD, MPH, CPE